LATE PREGNANCY SCREENING OF MARES FOR PLACENTITIS
Placentitis is an infection of the placental membranes and is usually caused by bacteria that gain access through the mare’s cervix in late pregnancy. Although only seen in about four percent of total pregnancies, its effects can be devastating, leading to abortion, or birth of an extremely sick foal, which may or may not survive even with intensive care. Owners are often unaware that a mare has placentitis, and arrive at the barn in the morning to find she has aborted. An affected mare may bag up and produce milk unexpectedly early, and she may also have vulvar discharge.
Researchers have linked specific changes seen on rectal ultrasound exams of the placenta with placentitis, including thickening and separation of the placenta from the uterus, changes in the appearance of the fluids and reduced fetal activity. Experience has shown, however, that by the time the mare shows obvious signs it may be too late and treatment is often futile. Treatment usually includes broad-spectrum antibiotics, anti-inflammatories and in some cases, supplemental progesterone.
The results of two recent studies question whether routine ultrasound examination of all mares is warranted, however. In one study (Löf et al. 2010) of 333 mares, the thickness of the placenta near the cervix on an ultrasound exam in the last month of pregnancy was not able to predict whether placentitis was present. Only two in 13 mares in the study, whose placentas showed abnormalities on examination after foaling, had thickened placentas on the ultrasound exam.
Most of the mares with placentitis at foaling showed normal placental thickness on ultrasound. In another recent study (Carrick, et al 2010) screening ultrasounds showed thickened placentas a surprisingly high 72% of the time, yet only 34% of placentas had abnormalities at foaling. Mares were divided into normal and high-risk groups, with a high-risk mare being defined as having had repeated late term abortions, a stillborn or premature foal, a small-for-age foal, or a septic foal.
This study showed a benefit to screening selected mares. Regular ultrasound monitoring of the high-risk mares more than doubled the chance of a live foal for those mares, compared to their live-foal rate over the three previous seasons, This is presumably because mares were treated for placentitis when ultrasounds showed any abnormalities. In addition, the study did show that reduced fetal activity and abnormal fluid character were highly associated with poor fetal outcome.
So what do these studies tell us? There is definite value in regular late pregnancy monitoring of mares at-risk. We can intervene sooner and increase the chances of foal survival if we identify problems earlier. Monthly or twice-monthly ultrasounds of high-risk mares should begin in the fifth or sixth month. However, routine screening of all mares will undoubtedly lead to many false diagnoses, and medication of a large number of mares unnecessarily. Treatment is expensive and time-consuming, and in this age of increasing concerns about antibiotic resistance, not without concern.
For some owners, the possibility of saving one foal might make the expense of unnecessary treatment of several mares worthwhile. However, in most situations, selection of mares at-risk for screening would seem the best approach. Mares you should target include those that have had repeated late term abortions, previously delivered a stillborn or premature foal, a small-for-age foal, or a septic foal. CT
BLOCKED OVIDUCTS AS A CAUSE OF INFERTILITY
Breeders and veterinarians are sometimes faced with mares that fail to become pregnant despite excellent reproductive management, and for which no cause of infertility can be found. Recently oviduct blockage has been suggested as a cause of infertility in the mare, and treatment by laparoscopic application of a hormone to unblock the oviduct, has suddenly become a hot topic. But does oviduct blockage really occur in the mare, and if so, how commonly?
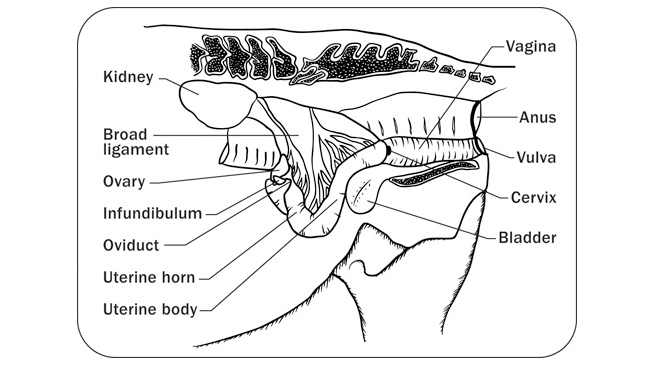
The oviduct, also known as the Fallopian or uterine tube, carries sperm from the uterus to the ovary, is the site of fertilization, and also carries the early embryo down into the uterus where it will spend the remainder of pregnancy. In one survey of reproductive tracts obtained at slaughterhouses, none of the 2,297 mare tracts had oviduct abnormalities. Yet in other reports, oviduct cysts, scarring and inflammation occurred in up to 50% of the specimens examined, with problems more frequent in tracts from old mares. Although common in women and cows, involvement of the oviduct due to infection moving upward from the uterus is rare in mares, due to the tight sphincter present at the junction of the oviduct and uterus. In mares, oviduct pathology would appear to be fairly rare.
The mare is unique in several ways with respect to her oviducts: her unfertilized eggs are retained within the oviduct; a large amount of follicular fluid passes into the oviduct due to the large size of her follicles at ovulation; and a hormone known as PGE2 (prostaglandin E) is secreted by the early embryo to help its transport down the oviduct and open the sphincter into the uterus. The discovery of the role of PGE2 has opened to door for potential treatments of blocked oviducts in mares.
Finding abnormalities of oviducts does not necessarily mean infertility, however. Fifty to 80% of mares with normal fertility have “plugs” in the oviduct, leading some researchers to speculate that they are a normal occurrence. The plugs are thought to arise from accumulation of eggs, mucous and follicular fluid over time. Could an excessive accumulation or hardening of these plugs, rather than scars or adhesions which are much more rare, become a physical obstruction and cause infertility? And if so, could they be flushed out or moved in some other way?
How to diagnose a blocked oviduct
Diagnosis of oviduct blockage is usually through a process of elimination. When a broodmare repeatedly fails to become pregnant and all other possible causes, including stallion fertility, have been ruled-out, one may become suspicious of oviduct blockage. Attempted embryo recovery may be informative, because if the uterine culture and biopsy are normal, breeding goes well and the stallion is of excellent fertility, failing to flush an embryo at seven days after ovulation is further presumptive evidence for oviduct blockage.
Workers in England (Allen et al 2006) used laparoscopic surgery to apply PGE2 to the oviducts of 15 infertile mares presumed to have blockages based on breeding history. Fourteen of the mares became pregnant either during the season of treatment or the following season, leading the authors to believe that successful treatment provided further evidence of oviduct blockage as the cause of the infertility. But there were no controls in this study – no barren mares left untreated and bred during the two breeding seasons, to compare pregnancy rates with. So we don’t know how many of those 15 mares would have become pregnant anyway, without surgery. Nevertheless, the study potentially identifies a treatment for that small group of mares with otherwise unexplained infertility.
Unfortunately application of PGE2 onto the uterine-tubal junction directly via the uterus is not effective. It must be applied onto the oviduct through a surgical approach. This makes treatment somewhat risky and expensive.
Is oviduct blockage a bona-fide cause of infertility in mares? Maybe….in a low number of mares for which a full range of tests are otherwise normal. The risks, cost and invasiveness of a flank laparoscopic surgery for application of PGE2 need to be considered. There are many other far more common causes of infertility that must be ruled out before you should consider sending your barren mare for surgery to apply PGE2 to potentially unblock her oviducts.
PROGESTIN SUPPLEMENTATION
Background
In early pregnancy, progesterone (P4) is produced in the ovary by the corpus luteum (CL ), which forms after ovulation. Some of the circulating P4 is further modified in the body to make other hormones (known as progestins) to support the developing foal. The ovary produces P4 until 120-150 days of gestation. By this time, the job of pregnancy maintenance has been taken over by the placenta, which produces P4 and other progestins. In fact, the ovaries are no longer necessary for pregnancy maintenance and as early as 70 days gestation could be removed in most mares without causing abortion.[1] By the second half of pregnancy, P4 itself is virtually undetectable in the mare’s circulation and other progestins are predominant.
Rationale
Breeders may face substantial financial and emotional losses due to pregnancy failure in the mare. Progestin supplementation is widespread throughout the industry in the hope of reducing these losses. But is there a valid medical rationale, or do we supplement because it makes us feel better?
Inherent failure of the CL to produce adequate P4 is rare. More often, the integrity of the CL is compromised by prostaglandin (PGF2) release from the uterus, which causes the CL to regress and stop secreting P4. Inflammation or infection in the uterus will induce prostaglandin release and thereby the demise of the CL . These uterine conditions should be treated and progestin supplementation is contraindicated.
If your mare suffers repeated early embryo losses without signs of uterine inflammation, a blood sample can be submitted to check progesterone levels after she ovulates. Though somewhat arbitrary, and it may vary for each individual, the rule of thumb is that a progesterone level of 4 ng/ml is sufficient to maintain pregnancy. If you discover a need for additional progestins, continue supplementation until accessory CL ’s form (recheck P4 levels around 50-60 days gestation) or until the placenta has taken over at 120-150 days, then wean her off over the next couple of weeks. Altrenogest (Regu-Mate®) is not recognized by most progesterone tests, so if you’re using this, you can still determine how much P4 your mare is producing herself. This can help you to determine when it’s safe to stop supplementation. In this regard, there is no good reason to check P4 levels after 80-100 days, since it will be diminishing and no longer accurately reflects the hormonal support available to the unborn foal.
In order for the CL to remain active beyond the length of a regular cycle, the embryo must make its presence known. The mechanism by which the embryo signals the mare is poorly understood. While there is likely to be some unidentified factor that the embryo must produce (as happens in other mammals), it is known that the embryo must be able to move freely throughout the uterus during the first couple of weeks of gestation. Defects in the embryo, in the recognition mechanism of the uterus, or impaired embryo movement (by large clusters of uterine cysts, for example) could conceivably cause failure of recognition of pregnancy. If the problem is not detrimental to the embryo, progestin supplementation might help to overcome this critical stage and allow continued development. Again, you would supplement until accessory CL ’s form, or until the placenta takes over. The actual incidence of failure of recognition of pregnancy as the cause of embryo loss is unknown.
Inadvertent administration of prostaglandin (e.g. Lutalyse® or Estrumate®) will also cause failure of the CL , loss of P4 and embryonic death. Starting supplemental progestins as soon as possible will allow continued development of the embryo until the placenta takes over progestin production (you may be successful starting as late as 4 days after the mishap [2]). This is the one instance where no discussion is necessary. Give the progestins if you want to save the pregnancy. That said, after about 40 days gestation accessory CL ’s have formed and it typically would take several injections of prostaglandin to debilitate all CL ’s.
Mares sustaining major injury, undergoing surgery or with general illness (such as colic or pneumonia), or with placentitis (see 42) may be at risk for premature delivery. These or similar conditions may cause inflammation and prostaglandin release which may threaten the CL (a problem in early pregnancy) or cause uterine contractions (a problem at any stage).
Though information in the literature is conflicting, it is generally believed that one of the roles of progestins is to inhibit uterine contractions. Progestin supplementation during the later stages of gestation (after the CL is no longer important for pregnancy maintenance) is aimed at preventing premature labor. Progestins are often included in the treatment plan for mares at risk despite the lack of controlled studies showing that supplementation improves the outcome. If the placenta itself is compromised to the point that it can no longer sustain the foal, no amount of progestin supplementation will help. Progesterone measurement in the late stages of pregnancy in mares at risk is sometimes performed to help assess the wellbeing of the foal. Depending on the type of compromise, progesterone levels might increase over several days or weeks if the fetus is stressed. If your mare is at risk and being treated already, this information is unlikely to change your treatment plan.
Forms of supplementation and side effects
Progestin supplementation can be given by intramuscular injection (progesterone), which may cause injection site reactions, or by daily oral administration of altrenogest (Regu-Mate®), which must also be handled with caution. Interestingly, Regu- Mate® is not labeled for use in pregnant mares and any such supplementation is an off-label use of the drug. The label does, however, include information on the outcomes of two controlled studies in which altrenogest was administered to pregnant mares.
These and other studies have shown that altrenogest treatment up until the time of foaling can affect both the foalingprocess and the newborn foal. It crosses the placenta and can be found in fetal fluids and in the circulation of newborn foals.[4]
Mares treated with altrenogest may foal earlier after treatment is discontinued than they would have if left untreated. Additionally, second stage labor was longer in mares treated with altrenogest up until foaling and foals showed decreased respiration and changes in the immune system and a higher incidence of problems in early life.[3] Studies in which altrenogest administration was discontinued at day 320 or 325 were shown
not to have adverse effects on the foal.[5]
Another documented effect of long-term altrenogest treatment is an enlarged clitoris in female offspring, though their future fertility was not affected. Unless your mare is at risk, supplementation should stop several days before foaling.
Progestin supplementation also has effects on the production of other hormones and can have a negative feedback effect on the progesterone that the mare produces on her own.
Conclusions
Supplemental progestins can be beneficial under some circumstances, but administration without an apparent medical need or without scientific basis is unwarranted. There is a monetary cost involved and it may not be innocuous. The decision to supplement (or not) should be made on a case-bycase basis with your veterinarian and treatment of underlying reasons for supplementation should be addressed if possible. Supplementation just “because we can” does not constitute good medicine.
Dr. Tracey Chenier and Dr. Elizabeth Scholtz are Board-Certified Equine Theriogenologists, on faculty in the Reproduction Section at the Ontario Veterinary College, University of Guelph.
1. Holtan DW, Squires EL, Lapin DR, Ginther OJ. Effect of ovariectomy on pregnancy in mares. J Reprod Fertil Suppl 1979: 457-463.
2. Kastelic JP, Adams GP, Ginther OJ. Role of progesterone in mobility, fixation, orientation, and survival of the equine embryonic vesicle. Theriogenology 1987;27: 655-663.
3. Neuhauser S, Palm F, Ambuehl F, Aurich C. Effects of altrenogest treatment of mares in late pregnancy on parturition and on neonatal viability of their foals. Exp Clin Endocrinol Diabetes 2008;116: 423-428.
4. Palm FM, Schenk I, Neuhauser S, Schubert D, Machnik M, Schanzer W, Aurich C. Concentrations of altrenogest in plasma of mares and foals and in allantoic and amniotic fluid at parturition. Theriogenology 2010;74: 229-235.
5. Shoemaker CF, Squires, E. L., Shideler, R. K. Safety of altrenogest in pregnant mares and on the health and development of offspring. Equine Vet Sci 1989;9: 69-72.